
SCREENING & EARLY DETECTION
Breast cancer is sometimes found after symptoms appear, but many women with breast cancer have no symptoms. This is why regular breast cancer screening is so important. Learn more.
Breast Cancer Information
Sign & Symptoms
Facts & Statistics
Risk Factor
Screening & Early Detection
Diagnosis
Treatment
Self Exams
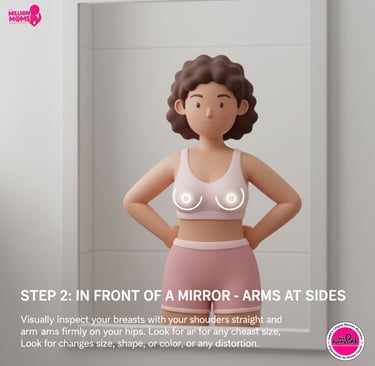
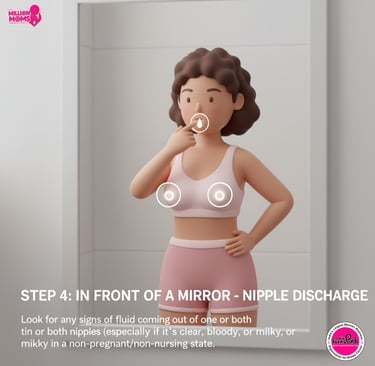
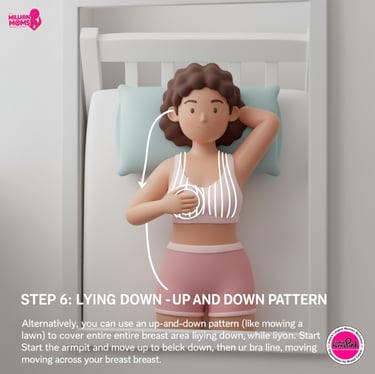
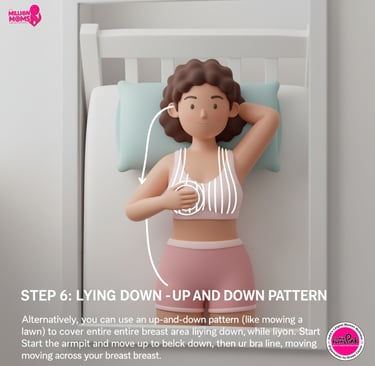
It’s a good idea to know how your breasts normally look and feel so you can notice any changes. India Turns Pink recommendations for Breast Self – Exams regularly.
For women at average risk, the American Cancer Society recommends that women ages:
– 45 to 54: Get yearly mammograms.
– 55 and older: Can switch to getting a mammogram every other year or continue getting yearly mammograms.
– 40 to 44: It’s OK to start a yearly mammogram.
India Turns Pink recommends screening mammograms every other year for women ages 50-74. The decision to get a mammogram every other year from age 40 to 49 is up to you and your doctor.
Screening Recommendation
How Do Doctors Diagnose Breast Cancer?
The only way to confirm cancer is for a doctor to do a needle aspiration or surgical breast biopsy to collect and test tissue for cancer cells.
If It’s Cancer
If you’re diagnosed with breast cancer, you and your doctor will need to know what type it is and how advanced it is. A check of your lymph nodes can tell if the disease has spread. Other tests give an idea of what treatments may work best for you, and still others predict the likelihood that your cancer will come back after treatment.
Your doctor can help you understand all of these tests, and together you’ll decide on the best treatment plan for you.








Breast Cancer Screening with India Turns Pink
India Turns Pink is India’s largest women’s wellness and breast cancer awareness movement, dedicated to early detection, education, and empowerment of women. For over a decade, we’ve been working tirelessly to make breast cancer screening accessible, affordable, and stigma-free across urban and rural India.
Why Choose India Turns Pink for Screening?
Choosing India Turns Pink means choosing trust, technology, and compassion.
Here’s why thousands of women prefer our screening programs:
Non-invasive & Painless: Our screening uses advanced technology like the iBreast device — no discomfort, no fear.
Radiation-free & Safe: Unlike mammography, iBreast is 100% radiation-free, safe for all age groups.
Affordable & Accessible: We bring screenings to schools, workplaces, villages, and cities — ensuring no woman is left behind.
Expert Team: Our programs are led by trained health professionals and supported by renowned oncologists.
Confidential & Supportive: Every woman is treated with dignity, privacy, and care.
About the iBreast Device
The iBreast device is a breakthrough handheld tool designed for early breast cancer detection. It uses advanced tactile sensing technology to detect tissue abnormalities — mimicking the sensitivity of a clinical breast examination but with greater accuracy.






Portable: Perfect for community and rural outreach programs.
No Radiation, No Pain: A safe, simple alternative to mammograms.
Instant Results: Screening results are available immediately.
Accurate & Reliable: Helps identify early-stage changes in breast tissue.
Key Features:


